|
The study’s authors remind us that nothing in the body acts in isolation, something we’ve long known in functional medicine and functional neurology.
Understanding some brain basics helps you understand symptoms when your brain isn’t working right. The brain is our heaviest and most complex organ, using most of the body’s oxygen and about 30 percent of its energy supply. The brain is divided into sections, each in charge of different functions although all working together. In functional neurology, we can identify areas of poor brain function and help you get them working better again with customized therapy and rehabilitation. Frontal Lobe The frontal lobe is the area of your forehead that stretches between the temples. The human frontal lobe distinguishes us from other animals and governs much of our personality, impulse control, and the ability to reason. A frontal lobe injury can completely change your personality and ADHD is understood to affect the frontal lobe. The frontal lobe also governs emotional drive, motivation, and planning. Poor frontal lobe function can result in an inability to set goals or follow through on projects or plans. You may feel lazy, unmotivated, or depressed if so. In fact, depression is simply a frontal lobe impairment. The frontal lobe activates the muscles. Poor frontal lobe function can result in moving more slowly or not swinging your arms when you walk. Fine-motor coordination also falls under the frontal lobe’s duties. This is needed for handwriting, embroidery, and other detailed movements of the hands. As the frontal lobe degenerates it’s typical for handwriting to worsen. Symptoms and signs of possible frontal lobe impairment
The temporal lobes are located on either side of the brain above the ears. They govern hearing, speech, memory, emotions, and distinguishing smells. Tinnitus (ringing in the ear) is a common symptom of temporal lobe dysfunction, although not all tinnitus is due to temporal lobe degeneration, as is difficulty distinguishing between different tones. Within the temporal lobes is the hippocampus, the seat of learning and memory. Degeneration of the hippocampus leads to poor memory and eventually Alzheimer’s disease. It is also involved with spatial orientation, sense of direction, and circadian rhythm (sleep-wake cycle). Symptoms and signs of possible temporal lobe impairment
The parietal lobes are located behind the ears and perceive and interpret sensations such as touch, pressure, texture, weight, size, or shape. The parietal lobe function also tells the body where it is in its environment. Reoccurring injuries are common with parietal lobe impairment. Symptoms and signs of possible parietal lobe impairment
Cerebellum Your cerebellum is two lobes at the back of the head, directly above your neck. It calibrates muscle coordination and balance and filters information before sending it to the brain. Symptoms and signs of possible cerebellum impairment
The occipital lobe is in the back of the brain and processes visual information. Symptoms of possible occipital lobe impairment
The good news is the brain is very receptive to improving with the right nutrients and input. Functional neurology excels in identifying areas of brain dysfunction and customizing brain rehabilitation specifically for your brain. Ask my office for more information. You can contact our office at 317-848-6000 or contact Dr. Ralston directly at [email protected]. Back pain complaints are often met with instruction to build up your core strength, and indeed this is important for better stability and protection for your back. But building core strength helps in another important way — it activates areas of the brain that can enhance stability, reduce pain, and naturally improve posture.
When many people think of the core, they think of six-pack abs we see on gym posters. But the core is basically the entire trunk of your body. The core includes the:
Many people develop chronic back pain because of a undiagnosed brain imbalance. The brain coordinates with the eyes and the inner ear to perceive where it is in relation to the environment. When that information is incorrectly interpreted due to a brain imbalance, the brain may believe the body is falling forward or backwards. To compensate, it adjusts the posture to lean in the opposite direction of the perceived fall. This all happens without a person’s conscious awareness, and can start in infancy. This constant over correcting creates not only bad posture, but also areas of muscular weakness and tension that affect the spine and other parts of the body, often resulting in chronic pain. These people may also find standing for a short length of time causes fatigue and back pain. It’s also not uncommon for people with this issue to struggle with anxiety — the constant sense of falling is a source of chronic stressor that can manifest as anxiety, fatigue, and mood swings. People often report a reduction in back pain and better posture when they take on a core strengthening program. Although strengthening and stretching the core muscles is a vital part of that rehabilitation, it also exercises the midline cerebellum, the area of the brain responsible for, among other things, movement, coordination, and posture. By repeatedly activating the core muscles, you are stimulating this part of the brain. How do you know if brain imbalances play a role in your back pain or posture, and whether core exercises can help you? The best way is to conduct your own field sobriety test — that’s right, the same one cops give to suspected drunk drivers. This is because being drunk also affects the cerebellum. It’s not uncommon for people with posture and back pain issues to also have poor balance due to a cerebellar issue. A core strengthening program should emphasize good form so you don’t risk injuring yourself. It should also include attention to stability and alignment. A brain imbalance will often cause a person to stand or lie crooked when they think they are straight because the brain is incorrectly perceiving the body’s position. Pilates is one excellent core strengthening technique that incorporates these strategies along with mindfulness and breath work, which are also great brain rehabilitators. If you have back pain, poor balance, anxiety, mood issues, gut problems, a previous brain injury, or other symptoms, a functional neurology rehabilitation protocol may be the vital boost you need. Many times when people get stuck on a functional medicine protocol, it’s because a brain-based issue is promoting inflammation and metabolic imbalances. Ask my office for more information on how we can help you achieve better brain health. You can reach us at 317-848-6000 or contact Dr. Ralston directly at [email protected]. You don't have to receive a blow to the head to suffer from brain injury. In fact, you can even injure your brain while wearing a helmet. This is because brain tissue is very delicate - the consistency of soft butter or egg white - and floats inside a skull lined with hard ridges. Impacts to the body, falls, and neck injuries are all it takes to injure the brain, especially if they happen repeatedly.
Here are some ways you can sustain a brain injury without ever hitting your head: Hard falls: When you fall your brain slams into one side of your skull and then the other. People who engage in activities that involve falling and crashing regularly (football, extreme sports, roller derby, etc.) should be aware of signs of brain injury, even if they wear a helmet. Body slams (such as in contact sports): Likewise, full impact hits to the body knock the brain around inside the skull. Landing on your tailbone: Although landing on your tailbone results in a sore bum, your brain is also victim to the force sent up the spine. Whiplash: Whiplash is a double whammy to the brain, which is why car accidents can be so devastating even if you didn't directly injure your head. Not only does the whiplash send the brain crashing back and forth inside the skull, but the shearing and twisting forces in the neck can also damage the brain stem. The brain stem may look simply like the connection between the brain and the neck, its an extremely important center of brain function. Damage to the brain stem can cause anxiety, insomnia, extreme moodiness, gut problems, autonomic problems, and extreme sensitivity to light, sound, and crowds. Falls and crashes also damage the fragile inner ear, or vestibular system, which plays a vital role in brain function and integrity. The reason football players and extreme athletes are making headlines is because repeated impacts to the body and head continually inflame and damage the brain, overwhelming its ability to recover until it eventually succumbs to dementia and Alzheimer's. Brain injury increases risk for more brain injury One of the most prominent signs of brain injury is worsened balance and coordination. Unfortunately, these symptoms predispose a person to further injure their brain due to increased clumsiness. Just one concussion increases the risk of a second by 150 percent. After two concussions, your risk for a third goes up by 300 percent. This is why it's so important to seek functional neurology and functional medicine interventions right away when you suspect you have injured your brain. Poor brain health increases brain injury risk It's not just how many times your brain slams around inside your skull that matters, but also the general health of your brain prior to injury. This is why some people recover more quickly from injury than others. If you eat fast foods regularly, are deficient in vital brain nutrients - such as essential fatty acids and vitamin D have undiagnosed food sensitivities (especially to gluten), or suffer from hormonal imbalances or deficiencies, your brain is going to fare more poorly after an injury. Because inflammation in the brain does not have an "off switch" the way it does in the body, brain inflammation is like a slow moving fire that can damage tissue for months and even years, causing symptoms long after the insults. The good news is that for all its fragility, the brain is an amazing organ when it comes to recovery and repair. It will eagerly respond to functional neurology and functional medicine protocols to improve function, dampen disorders, and enhance its overall integrity. Ask my office how we can help you get back your brain health and function. You can call us at (317) 848-6000 or you can contact Dr. Ralston directly at [email protected]. We are increasingly learning the effects of traumatic experiences on the brain, and now, newer research shows these effects can be passed on to children's genes. Research of Holocaust survivors showed that compared to control groups, their children exhibited genetic changes that increased the likelihood of stress disorders.
Other research shows post-traumatic stress disorder, or PTSD, can be passed on to offspring. Plus, most trauma survivors are coping with the neurological effects of PTSD as they raise their children, which greatly shapes a child's environment and responses to stress. In functional neurology, we frequently work with the neurological fallout of PTSD, which can include not only being triggered to re-experience the trauma, but also heightened stress response, sensitivity to light, sound, and crowds, emotional instability, depression and suicidality, anxiety and insomnia, disassociation and numbness, and addiction. How PTSD manifests depends on the person, and women's symptoms differ from men's. Men are more prone to anger and addiction whereas women struggle more with depression, anxiety, and health ailments. Trauma turns on and off genes in offspring In the Holocaust study, researchers discovered genetic differences in offspring of survivors. This finding upended traditionally held notions that environment and experience don't affect DNA in sperm and eggs of parents. Although it has long been believed conception delivers a genetic "clean slate," newer science on epigenetics shows that our environment and experiences constantly modify genes, even in egg and sperm. They found chemical tags on the DNA that regulates stress hormones in Holocaust parents and their children that were not found in the control group. However, they are not sure how those tags get passed on. Is PTSD inherited? Studies on whether PTSD is genetically inherited are not yet conclusive, although one study found genetic links in almost 30 percent of European-American women with PTSD. Understanding how big a role genetics plays in trauma would further understanding of why some people get PTSD when others don't, and how best to treat it. Also, researchers point to the fallout for children raised by adults with PTSD, which can perpetuate the disorder. Functional neurology and PTSD PTSD causes structural changes to the brain. The disorder shrinks some areas of the brain while enlarging others, keeping a person trapped in a neurological prison of hyper arousal, stress, and fear. For instance, the ventromedial prefrontal cortex shrinks, predisposing one to extreme fear and anxiety. PTSD also shrinks the hippocampus, the area responsible for learning and memory. On the other hand, the amygdala, the area that governs the fear response, enlarges. Compromises in these and other areas of the brain result in an easily triggered and over exaggerated fear response that can be exhausting and debilitating to the sufferer. Fortunately, the brain is very responsive to rehabilitation and PTSD sufferers can find considerable relief without drugs. In functional neurology, we use specific exercises and activities to dampen areas of the brain that are over responsive to stress and stimulate those areas that can help control the fear response. Contact my office for more information at 317-838-6000 or you can contact Dr. Ralston directly at [email protected]. When something stressful happens, our body goes into "fight or flight" mode, pumping out stress hormones, raising blood pressure and pulse, and shunting blood away from the organs and towards the limbs. When the stress is over, a healthy body bounces back and returns to normal.
Unfortunately, many people are stuck in fight-or-flight mode. This is especially true in people dealing with a chronic health or brain disorder, as their health itself is a chronic stressor in a self-perpetuating vicious cycle. The autonomic nervous system, which runs such bodily functions as digestion, heart beat, breathing, etc., consists of two arms: - The sympathetic system, also known as the fight-or-flight system. - The parasympathetic system, also known as rest-and-digest system. When you're in a life-or-death situation, you don't need to digest, detoxify, or regenerate cells - duties for the parasympathetic rest-and-digest system. The priority is simply to keep you alive. Once you're safe, the parasympathetic system kicks back in. The problem is modern life has many of us on hyper drive, in what feels like an ongoing attack. This keeps us in sympathetic mode longer than we should be. Causes of chronic fight-or-flight mode It's not just daily stress that can keep a person stuck in sympathetic mode. It could be stress from the past that has been hardwired into your brain, a concept referred to as negative plasticity. The neuron pathways in your brain have become highly efficient at stress so it takes less and less to trigger a stress response. The most common example of this is post-traumatic stress disorder, or PTSD. It can also come from long periods of overwork and sleep deprivation that have essentially trained your brain to be agitated all the time, even though your health is being sacrificed. Signs of chronic sympathetic stress Signs you are stuck in sympathetic mode include problems with sleep, anxiety, blood sugar issues (even with a blood-sugar-balancing diet), sexual dysfunction, brain fog, memory issues, fatigue, difficulty recovering from exercise or stressful events, getting sick easily, and chronic pain. Chronic sympathetic stress not only creates negative plasticity, it also damages the gut lining, leading to intestinal permeability, or leaky gut. This allows undigested foods, bacteria, yeast, and other pathogens into the bloodstream, where they trigger inflammation. This chronic inflammation is the foundation to many health maladies. Getting out of chronic sympathetic stress mode The most obvious first step to managing sympathetic stress is to address the cause of stress. The cause can be metabolic, such as chronic infection, blood sugar issues, hormone deficiencies, inflammation, or undiagnosed autoimmunity. Or it can be lifestyle, such as a toxic job or relationship, not sleeping enough, or taking on too much to do and never taking time off. Another commonly overlooked cause is a brain-based disorder. The less healthy or more degenerated the brain is, the less able it is to dampen sympathetic stress. If you suffer from brain fog, memory loss, poor cognitive skills, and lack of brain endurance, you may also find you're often in fight-or-flight mode. Problems with your vestibular (inner ear) system or cerebellum, both of which play a role in balance, can cause chronic sympathetic stress because the brain is constantly feeling unbalanced. People may also have issues with the basal ganglia - which acts as the gas and brake pedal of the brain - that keeps them chronically stressed out. These are just a few ways in which a brain-based disorder can contribute to sympathetic stress. In functional neurology we look at all facets of health to help you unwind sympathetic stress. Sometimes the issue can be as simple as removing certain foods from your diet that are inflaming your body and brain, gluten being the most common. Other times it takes a neurological exam and some sleuthing to determine whether the issue is brain-based. Often it is a combination of metabolic and brain-based causes. Ask my office how we can help get you out of chronic sympathetic stress and into a more balanced neurological state that includes plenty of restful and restorative parasympathetic activation.You can contact Dr. Ralston directly at [email protected]. 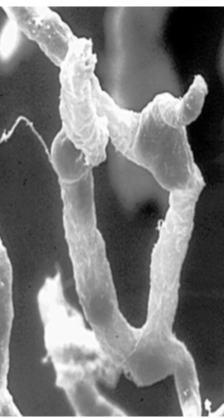 It has been a hundred years since a Nobel Prize winner discovered the thin barrier that surrounds and protects brain. Since then, we've learned this mesh of tightly joined cells, called the blood-brain barrier, is highly selective in a healthy person. It allows the transport of compounds back and forth through an intricate transport system while keeping out most everything else in the blood stream that can damage the brain. This includes heavy metals, toxic proteins, pathogens, and red and white blood cells. Accelerated aging + Inflammation = Leaky Brain Now, scientists have discovered that brain degeneration weakens the blood-brain barrier and causes it to "spring leaks." This is especially true in the hippocampus, the area of the brain associated with learning and memory. This discovery adds to the growing evidence that diseases of aging such as dementia and Alzheimer's are sometimes linked to what functional medicine practitioners call a "leaky brain." Researchers studying the brains of people with Alzheimer's disease have found significant amounts of compounds in the brain that a healthy blood-brain barrier should have kept out. Since not every aging person develops cognitive impairment, scientists theorize that the leaks are more extensive in some people than others. They also believe that some other phenomena, such as inflammation or pathogens, may be involved. Most research points to inflammation. Recently, biologists in the UK found that a molecule called microRNA-155, which is elevated in inflammation, creates gaps between the cells of the blood-brain barrier. They also found that the same molecule is elevated in inflamed brain areas of patients with multiple sclerosis. Even brain conditions such as depression, anxiety, brain fog, and various neurological symptoms are linked to body-wide inflammation, which often starts in the gut. This is Leaky Gut, Leaky Brain A "leaky gut" allows bacteria and toxic molecules to pass through an overly permeable gut lining into then bloodstream. This causes inflammation throughout the body, and a leaky brain is often one unfortunate consequence. Other inflammation triggers that contribute to a leaky brain are gluten sensitivity and similar food intolerances, out-of-control blood sugar, and too little thyroid hormone. Injury directly to the brain itself, such as in concussion, can also spark inflammation that damages the blood-brain barrier. Repairing leaky brain with functional nutrition You can protect your brain in part through various functional medicine strategies. This includes supporting the metabolic health of the brain by managing blood sugar, supporting gut health, addressing infections and toxicity, and following an anti-inflammatory diet. Nutritional compounds that support repair of leaky gut also help repair leaky brain, as do compounds targeted at quenching brain inflammation. Brain-saving nutrients include:
Is your brain on fire with inflammation? The brain doesn’t hurt like an inflamed knee does, so it’s hard to know if inflammation is happening. However, the brain communicates inflammation in how it makes you feel. One of the most common symptoms of brain inflammation is brain fog, that feeling of slow and fuzzy thinking. Other common brain inflammation symptoms include depression, anxiety, irritability, anger, memory loss, and fatigue. Even getting a song stuck in your head is a symptom. Of course, other factors can cause these symptoms, but an inflamed and thus quickly degenerating brain is often involved in brain-based symptoms. For instance, if these symptoms arise after eating certain foods, such as wheat or dairy, that can be a strong clue brain inflammation is at work.
Why inflammation causes brain fog One of the most common symptoms of brain inflammation is brain fog. Why is this? Inflammation in the brain slows down firing between neurons. Thus the overall operation of the brain slows down. This is what causes your brain function to be foggy, dull, and slow. In the case of depression, inflammatory immune cells called cytokines hamper brain function and the activity of serotonin, a brain chemical needed to feel joy and well-being. For example, depression is a common side effect with the anti-viral drug interferon, which raises cytokine levels. Also, brain imaging and autopsies show brain inflammation is more common in individuals with autism. It’s important to take brain inflammation seriously — inflammation in the brain damages and destroys brain cells, speeding aging and atrophy of your brain. This raises your risk for dementia, Alzheimer’s (brain inflammation increases amyloid beta), Parkinson’s and other degenerative brain diseases. Why does brain inflammation happen It’s very important to know why your brain is inflamed because this will point you in the right direction to address it and relieve symptoms. One of the more common causes of brain inflammation is an injury to the head. A brain injury causes the brain’s immune cells, which are different from those in the body, to begin the healing process and removal of dead and damaged neurons. However, immune cells in the brain do not turn off, especially if there are already other imbalances in the body. This means inflammation in the brain can continue long after injury. This is one reason football players have brain-related issues long after they retire. Other causes of brain inflammation include:
Brain inflammation means your brain is degenerating (aging) too fast. Brain-saving tips include: Take flavonoids, plant compounds that have been shown to reduce brain inflammation.
How your inner ear can influence your emotions
We tend to think of our emotions as being strictly tied to our psychology and personality — some people are highly emotional and others are not. But did you know your inner can profoundly affect your emotions? Our inner ear, called the vestibular system, is integrated with the eyes and the brain to tell you where you are in space and is integral to survival, safety, and attention. This system is a labyrinth of the semi-circular positioned in right angles to each other so they can perceive motion in three-dimensional space. You engage your vestibular system when you turn your head, change positions, look one direction while moving in another, balance on one leg, ride a bike, and so on. The vestibular system also plays a role in integrating gravity, acceleration, and deceleration. In summary, the vestibular system works with your eyes and your brain to keep your body stable and aware of where it is in the environment around it. Imagine driving while holding a glass of water and how accelerating, driving at an even speed, stopping, and turning affect the water in the glass. This is somewhat how the vestibular system, which contains fluid and sensory hair cells, works to deliver information to the brain. When the vestibular system isn’t working well Unfortunately, the inner ear can be quite fragile and vulnerable to damage from concussions, micro-traumas to the brain, and whiplash. Many people have vestibular system damage or disorders that they are not aware of. Some hallmarks of vestibular problems include poor balance, dizziness, and being easily prone to motion sickness. When the inner ear canals are damaged, information from the vestibular system does not coordinate properly with information from the eyes and the body. This causes neurological confusion and resulting symptoms. A poorly functioning cerebellum also plays a role in vestibular dysfunction. The cerebellum is the area at the base of the brain — it works closely with the vestibular system and is integral to balance and coordination. How inner ear problems cause emotional problems When your vestibular system is damaged, or when there is dysfunctional coordination between the inner ear and the cerebellum, your sense of balance and stability are affected. The body ultimately perceives this as a stressor. Typically, vestibular dysfunction is too subtle for most people to notice. Yet it nevertheless creates a sense of neurological confusion the brain and body perceive as chronically and subtly terrifying, thus putting the survival system on red alert and raising stress hormones. People who have experienced anxiety after being on a roller coaster or from spinning may understand this connection Emotions are governed by an area of the brain called the limbic system, and extensive networks exist between the vestibular and the limbic system. In fact, it’s not uncommon for people diagnosed with vestibular disorders to report they are not themselves emotionally. Rehabilitating the inner ear for healthier emotions Researchers are able to impact a person’s depression, anxiety, and other emotional states by activating and rehabilitating the vestibular system, lending further weight to the connection between the inner ear and emotions. Fortunately, functional neurology is well grounded in the examination of the vestibular system, identifying dysfunction, and creating customized exercises to help you rehabilitate your vestibular system and brain. This can bring not only relief from physical signs and symptoms, but it can also lower anxiety and relieve emotional symptoms. Ask my office for more information. |
NeuroHealth Services
|
Our Doctors |
Learn More |
|
|

 RSS Feed
RSS Feed
